Health
Study Reveals Risks of GLP-1 Use During Pregnancy
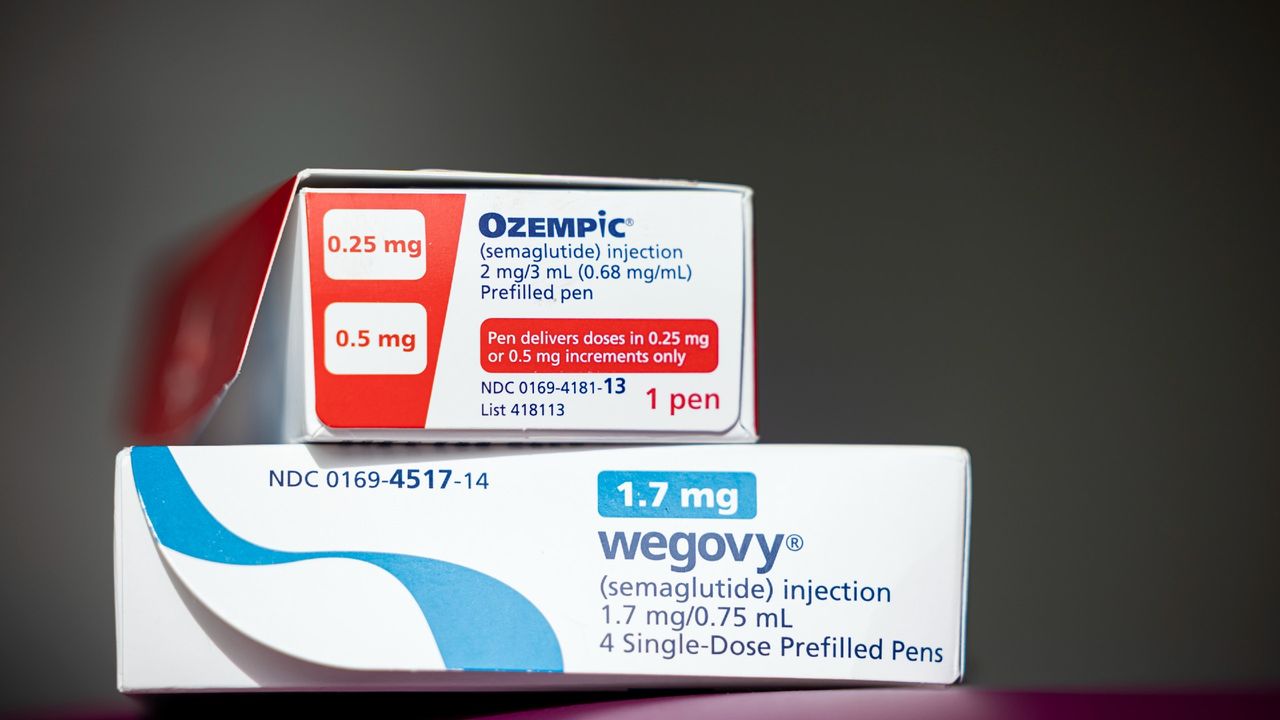
Recent research indicates that the use of GLP-1 medications, such as Ozempic, may be linked to certain pregnancy risks. However, the findings also suggest that discontinuing these drugs before conception could pose its own challenges. The study, which involved analyzing hundreds of pregnancies from the Mass General Brigham health system between 2016 and 2025, highlights the need for further investigation into the implications of GLP-1 usage in women planning to conceive.
Dr. Jacqueline Maya, a pediatric endocrinologist and lead author of the study, emphasized that while the data should be seen as an early warning, it comes with significant limitations. The research did not adequately compare the health outcomes of women who had used GLP-1 medications against those who had not, potentially skewing results. “We don’t know if there’s a benefit, or if there’s increased risk, if you get to pregnancy at a lower weight and then come off the medication,” she explained.
The GLP-1 drugs, which include Wegovy and Zepbound, have been effective in managing weight and improving blood sugar levels. They work by influencing several mechanisms, such as slowing digestion and changing hunger signals in the brain. Previous studies in animal models have raised concerns about potential risks, including birth defects and pregnancy loss associated with these medications.
Currently, the recommendation is for women to stop using GLP-1s prior to conception. However, this leads to a population of women who face the risk of weight gain and related health issues after discontinuing the drugs. The study found that women who had taken GLP-1 medications gained more weight during pregnancy compared to those who had never used them, with an average weight gain of about 30 pounds (13.7 kilograms) versus 23 pounds (10.5 kilograms) in the control group.
Among those who had previously taken GLP-1 medications, approximately 65% experienced excessive weight gain during pregnancy, in contrast to 49% in the comparison group. This excessive weight gain can increase health risks for both mothers and their babies, highlighting the need for careful monitoring of these patients during pregnancy.
The study also identified an increased risk of preterm delivery, gestational diabetes, and hypertensive disorders, such as preeclampsia, among women who had used GLP-1s. These findings underscore the complexity of managing weight and health before and during pregnancy, particularly for women who may have been prescribed these medications for obesity.
Despite the critical insights provided by this research, several limitations must be acknowledged. The study compared women who had taken GLP-1s with those who had never used them, focusing on their weight at the time of pregnancy. This approach did not account for the potential changes in weight experienced before beginning GLP-1 therapy. Future research aims to gather more accurate data on women’s pre-treatment weights to better assess the benefits and risks of GLP-1 use prior to conception.
The new findings, published in JAMA, are significant as they contribute to a growing body of evidence regarding the implications of GLP-1 medication use among women of childbearing age. There remains a critical gap in clinical guidance surrounding the use of these drugs during pregnancy, as initial clinical trials often excluded women planning to conceive.
“It is critical that we strive to generate the evidence needed both to inform obstetric care and guide treatment initiation decisions,” the commentary authors noted. As research continues to evolve, health professionals aim to advocate for vulnerable populations, ensuring that all patients receive tailored care based on the latest findings.
This article serves as a reminder of the importance of ongoing research in understanding the complexities of medication use during pregnancy and the need for healthcare providers to monitor patients closely in light of emerging data.
-

 Top Stories1 month ago
Top Stories1 month agoRachel Campos-Duffy Exits FOX Noticias; Andrea Linares Steps In
-

 Top Stories1 week ago
Top Stories1 week agoPiper Rockelle Shatters Record with $2.3M First Day on OnlyFans
-

 Top Stories6 days ago
Top Stories6 days agoMeta’s 2026 AI Policy Sparks Outrage Over Privacy Concerns
-

 Sports5 days ago
Sports5 days agoLeon Goretzka Considers Barcelona Move as Transfer Window Approaches
-

 Top Stories1 week ago
Top Stories1 week agoUrgent Update: Denver Fire Forces Mass Evacuations, 100+ Firefighters Battling Blaze
-

 Top Stories1 week ago
Top Stories1 week agoOnlyFans Creator Lily Phillips Reconnects with Faith in Rebaptism
-
 Top Stories5 days ago
Top Stories5 days agoWarnock Joins Buddhist Monks on Urgent 2,300-Mile Peace Walk
-

 Entertainment6 days ago
Entertainment6 days agoTom Brady Signals Disinterest in Alix Earle Over Privacy Concerns
-

 Top Stories1 week ago
Top Stories1 week agoOregon Pilot and Three Niece Die in Arizona Helicopter Crash
-

 Top Stories4 days ago
Top Stories4 days agoCBS Officially Renames Yellowstone Spin-off to Marshals
-

 Health2 months ago
Health2 months agoTerry Bradshaw Updates Fans on Health After Absence from FOX NFL Sunday
-

 Sports4 days ago
Sports4 days agoSouth Carolina Faces Arkansas in Key Women’s Basketball Clash



