Scientists Uncover How Glioblastoma Attacks Skull, Complicates Treatment
Researchers have made a significant breakthrough in understanding the progression of glioblastoma, a particularly aggressive form of brain cancer. For the first time, a study from the Albert Einstein College of Medicine and the Montefiore Einstein Comprehensive Cancer Center (MECCC) reveals that this deadly cancer not only invades brain tissue but also erodes the skull itself. This unique behavior may explain the ineffectiveness of current treatments.
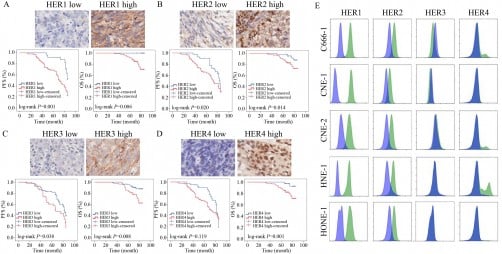
The findings, published in March 2024 in the journal Nature Neuroscience, highlight how glioblastoma interacts with the body’s immune system. Researchers observed two distinct types of glioblastomas in mice, noting that the tumors significantly altered the thickness of the skull, particularly in areas where bones fuse. This erosion is believed to create pathways for tumor cells to infiltrate bone marrow, thereby compromising the body’s immune defenses.
Jinan Behnan, an assistant professor at Albert Einstein College of Medicine and corresponding author of the study, emphasized the implications of this discovery. “Our findings suggest that current therapies, which treat glioblastoma as a localized disease, may fail because they do not consider its systemic nature,” Behnan stated. Glioblastoma, the most common type of brain cancer, poses a grim prognosis, with less than 7% of patients surviving beyond five years and a median survival rate of just 14.6 months for adults.
The research team’s investigation revealed that the erosion of the skull increased the number and size of channels leading from the skull to the bone. These channels could allow tumor cells to influence the immune environment in the skull marrow. The researchers utilized single-cell RNA sequencing to uncover changes in this environment, specifically noting an increase in pro-inflammatory neutrophils and a decrease in B cells, which produce antibodies against cancer.
Study co-author E. Richard Stanley, a professor of developmental and molecular biology, noted the implications of these findings. “The influx of pro-inflammatory cells from the skull marrow to the tumor renders glioblastoma increasingly aggressive and, unfortunately, often untreatable,” he explained. The research indicates a pressing need for treatment strategies that can restore the balance of immune cells within the skull marrow of glioblastoma patients.
Traditionally, treatment approaches have centered on the notion that glioblastoma is a localized condition. However, the latest findings suggest that the disease affects genes in skull marrow differently than in other areas, such as femur marrow. This distinction highlights the need for therapies that address the systemic nature of glioblastoma.
To explore potential therapeutic options, researchers administered anti-osteoporosis drugs, zoledronic acid and denosumab, to the mice. While both drugs successfully halted bone loss, the study found that zoledronic acid unexpectedly accelerated the growth of one glioblastoma variant. Additionally, both drugs interfered with the positive effects of the immunotherapy drug anti-PD-L1, which typically enhances the activity and production of tumor-fighting T cells.
This research marks an essential step in understanding why current glioblastoma treatments yield low success rates. By re-evaluating the disease’s progression and its impact on the immune system, scientists hope to pave the way for more effective, non-localized treatment strategies. The findings underscore the complexity of glioblastoma and the urgent need for innovative approaches to combat this formidable cancer.