Scientists Uncover Brain’s Sugar Mechanism Linked to Depression
Research from the Institute for Basic Science in South Korea has identified a potential new pathway for treating depression, linking a sugar-modifying process in the brain to mood disorders. The study reveals how chronic stress alters protein glycosylation, a process that may significantly influence depression-like behaviors.
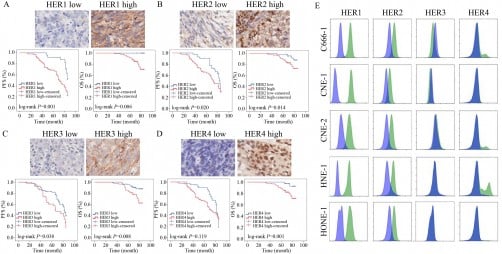
Chronic stress has been known to rewire the brain, contributing to various mental health issues. The researchers found that prolonged stress affects how proteins in the medial prefrontal cortex (mPFC) are modified with sialic acid, a sugar molecule essential for neuron function. This alteration is part of a process called glycosylation, which has gained attention for its roles in cancer and neurodegeneration but had not been thoroughly explored in mental health research.
The study highlights a specific type of glycosylation known as O-glycosylation. This involves the attachment of sugars to oxygen atoms on particular amino acids within proteins, creating a “sugar coating” that regulates neuronal communication. The researchers discovered that chronic stress disrupts these sugar patterns, potentially leading to impaired communication between brain cells.
Key Findings on Enzyme’s Role
The research team identified an enzyme named St3gal1 as crucial in the final step of O-glycosylation, which influences protein stability and synaptic interactions. When the expression of St3gal1 diminished in stressed mice, the final sugar-capping step was also reduced, resulting in behaviors associated with depression, such as loss of motivation and increased anxiety. Conversely, enhancing St3gal1 expression in stressed mice alleviated these symptoms.
Using high-performance mass spectrometry, the scientists mapped O-glycosylation across nine brain regions in healthy mice. Each region displayed distinct sugar signatures, reflecting its unique cellular characteristics. The most significant changes were observed in the mPFC, a critical area for mood regulation, underscoring the enzyme’s pivotal role in maintaining mental health.
Research fellow Boyoung Lee stated, “This study demonstrates that abnormal glycosylation in the brain is directly connected to the onset of depression. It provides an important foothold for identifying new diagnostic markers and therapeutic targets beyond neurotransmitters.”
Implications for Mental Health Treatment
The findings could pave the way for innovative approaches to treating depression and potentially other mental illnesses, such as PTSD and schizophrenia. Current antidepressants primarily target serotonin, but evidence suggests that depression involves more complex biochemical pathways than previously understood.
C. Justin Lee, director of the Institute for Basic Science, emphasized the societal impact of depression, noting that “this achievement could extend not only to depression therapy but also to other mental illnesses.”
Interestingly, the study also revealed gender differences in response to chronic stress. While male mice exhibited significant changes in St3gal1 levels, female mice showed behavioral alterations without corresponding changes in this enzyme. This discrepancy suggests that males and females may utilize different molecular pathways to cope with stress, offering another avenue for future research.
The research was published in the journal Science Advances, marking a significant advancement in understanding the biological underpinnings of depression. As scientists continue to explore this new direction, there is hope for the development of targeted therapies that address the underlying mechanisms of mood disorders, rather than merely alleviating symptoms.