NHS Launches Pilot for Innovative Cancer Detection Test in England
The National Health Service (NHS) in England is set to launch a pioneering pilot program utilizing a novel diagnostic tool known as the “sponge on a string” test. This initiative aims to identify early signs of oesophageal cancer, a condition that is often diagnosed at an advanced stage. The program is part of the government’s comprehensive 10-year health plan, which seeks to improve cancer detection and treatment across the nation.
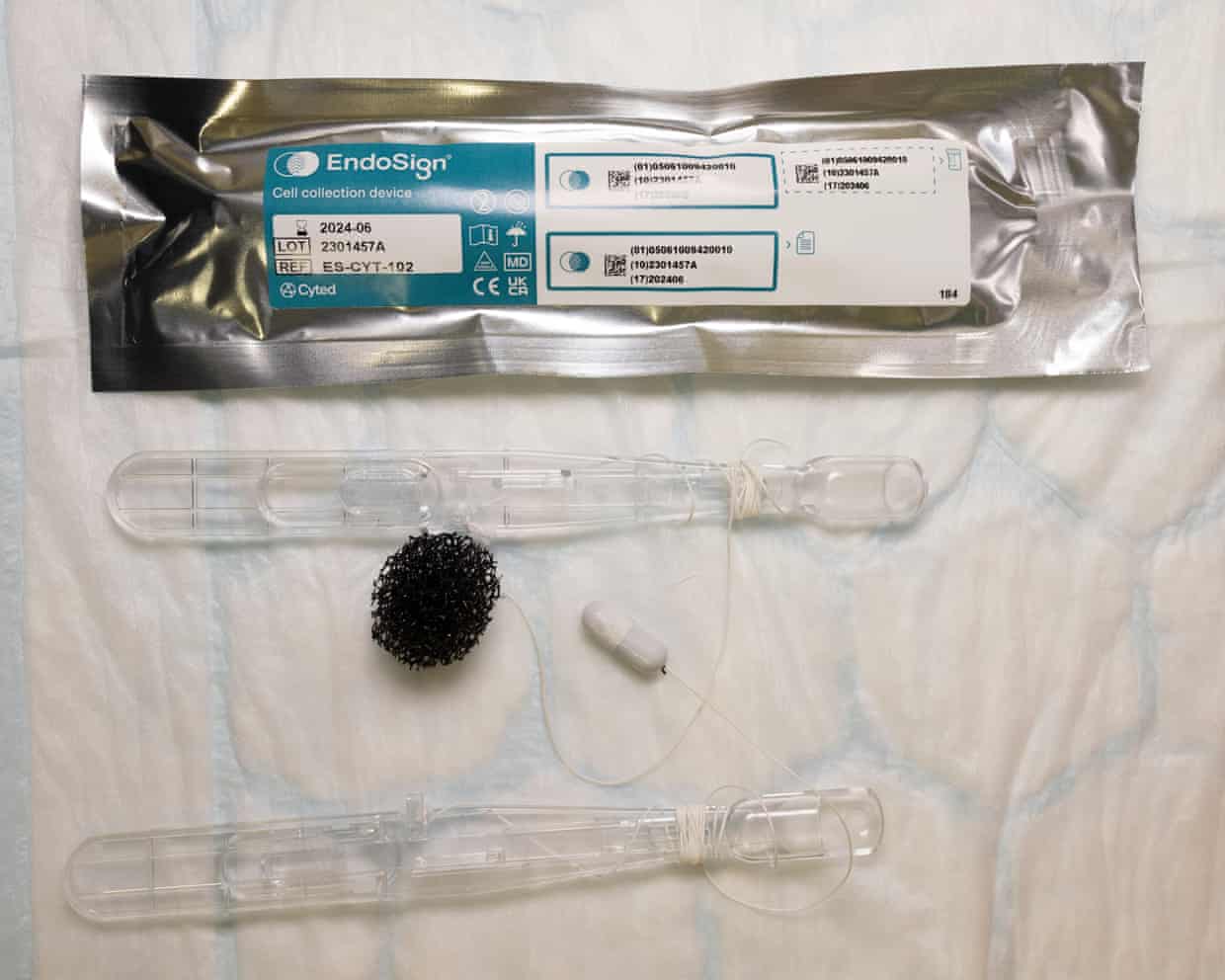
This innovative test involves a small sponge attached to a string that is swallowed by the patient. Once ingested, the sponge collects cells from the lining of the oesophagus. The procedure is designed to be quick and minimally invasive, allowing healthcare providers to gather critical information on potential cancerous changes. The pilot will take place across various NHS pharmacies in England, enabling easier access for patients.
Targeting Early Detection
Oesophageal cancer is one of the most challenging cancers to detect early, with survival rates significantly improving when the disease is identified at an initial stage. According to Cancer Research UK, around 10,000 people are diagnosed with this type of cancer each year in the UK. The pilot program is expected to enhance early detection efforts, potentially saving lives through timely intervention.
The initiative aligns with the broader objectives outlined in the government’s health strategy, which aims to reduce cancer mortality rates by 2032. The Department of Health and Social Care has expressed optimism about the pilot’s potential impact on patient outcomes. “We are committed to transforming cancer care in England. This innovative test could be a game changer in diagnosing oesophageal cancer earlier,” stated a spokesperson for the department.
Broader Implications for Cancer Care
The sponge on a string test represents a significant step forward not only for oesophageal cancer detection but also for cancer screening as a whole. By integrating this test into community pharmacies, the NHS is making cancer screening more accessible, particularly for individuals who might otherwise face barriers to traditional hospital visits.
Experts believe that such initiatives could lead to increased public awareness regarding cancer symptoms and the importance of early detection. The pilot program is expected to gather valuable data on the effectiveness of the test, which, if successful, could influence future cancer screening protocols.
As the NHS embarks on this pilot, the results will be closely monitored to assess the test’s reliability and its reception among patients. The outcome may have lasting implications for how oesophageal cancer is diagnosed and treated, reflecting a shift toward more proactive healthcare strategies in England.
Overall, this trial is a vital element of the NHS’s ongoing commitment to improving health outcomes and addressing the rising incidence of cancer. With an eye towards the future, the sponge on a string test could pave the way for transformative changes in cancer diagnosis and treatment, potentially shaping healthcare practices beyond England.






