Alzheimer’s Protein Boosts Immune Cells, Reduces Cancer Risk
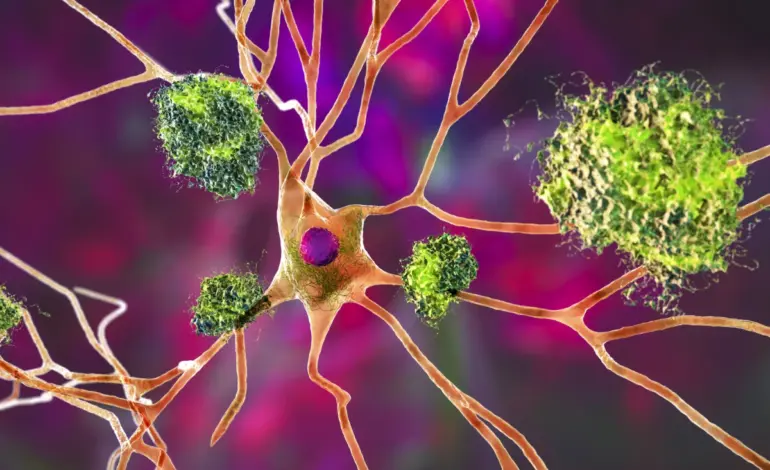
Recent research reveals that a protein commonly associated with Alzheimer’s disease may enhance the immune system’s ability to combat cancer. A study conducted by the Hollings Cancer Center at the Medical University of South Carolina (MUSC) found that a byproduct of amyloid-beta rejuvenates T cells, significantly increasing their effectiveness against tumors.
This discovery sheds light on the paradoxical relationship between Alzheimer’s disease and cancer. Previous studies have indicated that individuals diagnosed with Alzheimer’s are considerably less likely to develop cancer. The latest research aims to explore the underlying mechanisms of this phenomenon.
Dr. Besim Ogretmen, the associate director of Basic Science at Hollings and the study’s corresponding author, stated, “What we found is that the same amyloid peptide that is harmful for neurons in Alzheimer’s is actually beneficial for T cells in the immune system. It rejuvenates the T cells, making them more protective against tumors.”
Analysis of five years of nationally representative surveys revealed that adults over 59 with Alzheimer’s were an astonishing 21 times less likely to develop cancer compared to their peers without the disease. This prompted researchers to investigate the role of the amyloid-beta precursor protein (APP) and its breakdown product, amyloid-β 40, within T cells.
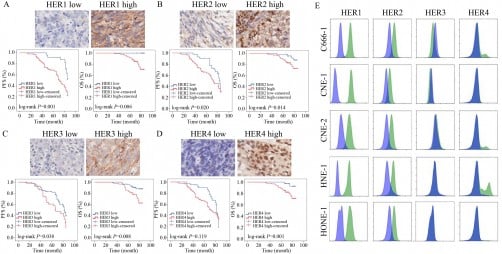
As T cells age, they often undergo a process called mitophagy, which is crucial for maintaining mitochondrial health. However, in aging T cells, this process can become overactive, leading to excessive mitochondrial loss and an impaired immune response. The researchers sought to understand how APP and its byproducts could mitigate this decline.
To explore this, the research team performed various experiments on both human and animal cells. They used genetically modified mice exhibiting Alzheimer’s-like features and compared their immune responses to those of non-Alzheimer’s mice. The team implanted cancer cells in these mice to assess tumor growth rates. They also transferred T cells from Alzheimer’s mice into non-Alzheimer’s mice to determine if these immune cells could influence tumor development.
The results were thought-provoking. In Alzheimer’s mice, APP and amyloid-β 40 were found to enter mitochondria, effectively blocking excessive mitophagy. This action preserved T cell health and functionality, resulting in slower cancer progression. Notably, even transferring T cells from Alzheimer’s mice to non-Alzheimer’s counterparts led to tumor shrinkage, indicating that the benefits were immune-driven.
The research revealed that aging T cells typically experience a loss of fumarate, an important metabolite for energy and mitochondrial function. This loss disrupts the chemical modification of proteins such as Parkin, which tags damaged mitochondria for destruction. APP’s presence prevented fumarate depletion, thus protecting mitochondrial integrity and enhancing T cell capabilities.
Dr. Ogretmen explained, “When you deplete fumarate, you increase mitophagy much more. Fumarate no longer binds proteins involved in that process, so the proteins become more active and induce more mitophagy. It’s like a reinforcing feedback loop.”
Importantly, introducing additional fumarate or healthy mitochondria into aging T cells replicated the cancer-fighting effects observed in Alzheimer’s cells, suggesting potential therapeutic avenues. T cells from older individuals exhibited similar patterns of excessive mitophagy and low fumarate levels. However, in T cells from older people with Alzheimer’s, these issues appeared to be resolved, resembling the functionality of younger T cells.
Dr. Ogretmen noted, “Older T cells began functioning like young, active T cells again. That was an incredible finding because it suggests a whole new way to think about rejuvenating the immune system.”
These findings not only clarify why individuals with Alzheimer’s are less prone to cancer but also pave the way for innovative therapeutic strategies. Targeting mitophagy, restoring fumarate levels, or modulating APP-related biological pathways could potentially revitalize aging immune cells and enhance cancer immunotherapy outcomes in older adults.
The full study was published in the journal Cancer Research in January 2024, marking a significant step forward in understanding the complex interactions between neurodegenerative diseases and cancer.