Research Reveals Why Women Face Higher Dementia Risks
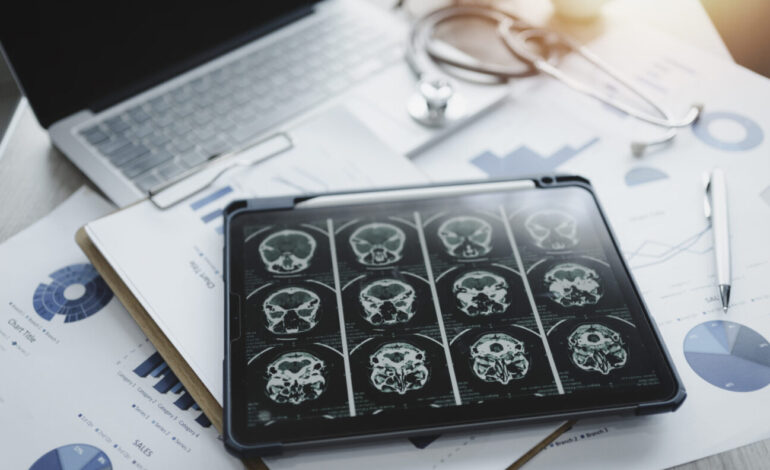
A significant new study has identified crucial factors behind the higher prevalence of dementia in women, particularly in the context of Alzheimer’s disease. Nearly two-thirds of Americans diagnosed with Alzheimer’s are women, and they often experience a more rapid cognitive decline than their male counterparts. Research led by Dr. Farida Sohrabji, a Regents Professor at Texas A&M University, has uncovered that biological sex plays a critical role in increasing the risk of stroke among older women, which in turn accelerates the onset of dementia.
In discussing the implications of her research, Sohrabji stated, “In every decade after 50, women are more likely to experience stroke compared to men, especially severe strokes.” This observation is vital as it highlights a significant contributor to cognitive impairment and dementia. The findings underscore the importance of developing targeted drug therapies and personalized medical approaches for women facing these health challenges.
Understanding the Hormonal Influence
The research team aimed to delve deeper into the reasons behind the disproportionate impact of dementia on women. One major discovery was the role of hormonal changes during menopause. As estrogen levels decline, the female brain becomes increasingly susceptible to inflammation and damage, known risk factors for dementia. Sohrabji noted, “We found estrogen appears to protect against stroke.” Initial studies showed that the removal of ovaries worsened stroke outcomes, but surprisingly, estrogen replacement did not yield the expected protective effects.
Sohrabji explained, “Estrogen was actually toxic. It made the loss of brain tissue more severe.” The complexity of the relationship between estrogen and brain health illustrates the need for nuanced approaches to treatment, particularly in older women.
Advancements in Sex-Specific Therapies
In light of the unexpected results regarding estrogen, Sohrabji and her research team explored the potential of a small peptide called IGF-1 (insulin-like growth factor) in conjunction with estrogen therapy. Their findings were promising; the combination not only mitigated the harmful effects of estrogen in older female models but also demonstrated that IGF-1 treatment alone could significantly improve stroke outcomes.
“If you gave the subjects estrogen and IGF-1, you clearly see neuroprotective effects,” Sohrabji remarked. The research indicated that IGF-1 is one of the most neuroprotective molecules tested, offering hope for tailored treatments that address the unique needs of older women.
Additionally, studies involving a non-coding RNA molecule produced similarly remarkable results. This agent not only protected brain tissue but also significantly reduced long-term cognitive decline in older female subjects compared to their male counterparts. “Our findings suggest the agent played a protective role in the process,” Sohrabji stated, emphasizing the importance of sex differences in brain research.
Sohrabji’s work reflects a broader shift in neuroscience and medicine towards recognizing the significance of biological sex in treatment strategies. By advocating for sex-specific research, she envisions a future where women no longer disproportionately bear the burden of Alzheimer’s.
The implications of this research extend beyond academic interest; they represent a crucial step toward improving health outcomes for women facing dementia. Sohrabji’s studies have been published in esteemed journals, including the Journal of Neuroscience, Brain Behavior and Immunity, and Neurobiology of Aging, with ongoing research available in preprint form at BioRxiv.
As the understanding of dementia evolves, Sohrabji’s work highlights the necessity of personalized, sex-specific therapies that can lead to better overall health outcomes for women.