New Injectable HIV Prevention Drug Promises Major Impact
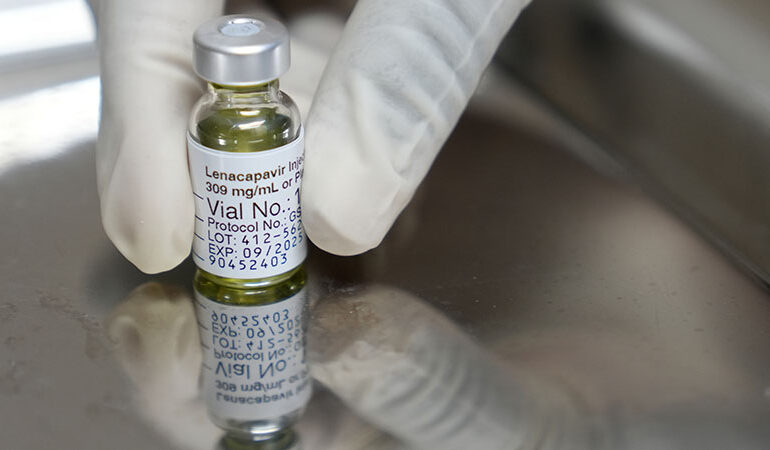
Advocates for HIV prevention are heralding the approval of a new injectable medication as a significant advancement in the fight against the virus. The U.S. Food and Drug Administration (FDA) recently approved lenacapavir, marketed under the brand name Yeztugo, following clinical trials that indicated the drug nearly eliminated HIV transmission among participants. Unlike traditional daily oral pre-exposure prophylaxis (PrEP), the new injectable treatment is administered just twice a year, promising to reduce barriers for those at risk.
Impact on HIV Prevention
“This new injectable PrEP for HIV prevention is going to be a major step forward for many individuals,” said Christopher Hamilton, CEO of Texas Health Action, a non-profit organization based in Austin dedicated to providing support for people living with HIV. The twice-yearly injection can significantly benefit those who struggle to adhere to a daily pill regimen.
Hamilton noted that individuals facing challenges such as unstable housing often find it difficult to store and consistently take medication. “You don’t have to remember to take a pill every single day,” he explained, highlighting the potential for improved adherence among vulnerable populations.
Currently, Texas Health Action’s Kind Clinic is developing protocols to offer the injection, although Hamilton indicated there is no set timeline for implementation.
Financial Concerns and Community Support
A major concern surrounding lenacapavir is its cost. Each injection carries a list price of over $14,000, and the extent of insurance coverage remains uncertain. According to NBC News, obtaining coverage for the injectable form may require a medical exception, necessitating detailed documentation from healthcare providers as to why this method is preferable to daily oral medications.
While daily oral PrEP is typically covered by most insurance plans, Hamilton anticipates that it could take time for insurers to assess the injectable version. “There is hope that prices will decrease over time, similar to what we witnessed when PrEP first entered the market,” said Eli Oldham, director of the Hill Country Ride for AIDS, an annual fundraiser that supports nine Central Texas non-profits focused on HIV/AIDS services.
Set to take place on April 18, 2026, the Hill Country Ride for AIDS has been instrumental in funding critical services over its 27-year history. Oldham expressed optimism that as the market evolves, the costs associated with lenacapavir may also become more manageable.
Hamilton further emphasized the importance of securing affordable access to the medication. He stated, “It will take time to determine the feasible pricing for organizations to absorb, but the manufacturer will offer a patient assistance program for uninsured individuals.”
In terms of administration, the injection must be administered by a healthcare professional, either in a clinical setting or a specialty pharmacy. “Fortunately, at Kind Clinic, we have pharmacies located within our facilities, allowing us to provide on-site administration,” Hamilton noted.
Clinical trials conducted by Gilead demonstrated lenacapavir’s effectiveness compared to daily PrEP options. Participants at risk for HIV, including gay and bisexual men and transgender individuals, received either the lenacapavir injection every six months or daily Truvada pills. The results indicated that lenacapavir was 89% more effective in preventing HIV transmission than its oral counterpart.
As the introduction of this new injectable treatment unfolds, Hamilton encourages individuals who have not yet established care to take action. “If you haven’t connected with a healthcare provider, now is the time. Know your status and prioritize your sexual health,” he advised.
For both Hamilton and Oldham, the arrival of this twice-yearly preventive injection represents more than just a medical breakthrough; it symbolizes hope for the future of HIV prevention. “Anytime there’s a breakthrough or new treatment for HIV, it’s exciting because it’s all about the progress we are making,” Oldham concluded.